For more information or for help finding a dentist practicing dental sleep medicine, click here.
Sleep Apnea and Snoring – Overview & Facts for Patients
[1] Resolution 17H-2017 passed by the ADA House of Delegates at ADA 2017, https://www.ada.org/en/publications/ada-news/2017-archive/october/sleep-related-breathing-disorder-treatment-outlined-in-new-policy
Snoring
You or your bed partner recognize snoring as the often loud or harsh sound that can occur as you sleep. As you breathe the flow of air makes the tissues in the back of your throat vibrate. The sound usually occurs as you breathe in air. It can come through the nose, mouth or a combination of the two. It can occur during any stage of your sleep.

Sleeping on your back may make you more likely to snore. It may also occur as your throat muscles relax from use of alcohol or other depressants. Congestion from a cold or allergies can also cause you to snore.
Of course, snoring can be a real nuisance to your partner and anyone else nearby. You may even snore loudly enough to wake yourself up! Though, in many cases people do not realize that they snore. Snoring can also cause you to have a dry mouth or sore or irritated throat when you wake up.
Light snoring may not disrupt your overall sleep quality. However, heavy snoring may be associated with obstructive sleep apnea, a risk factor for heart disease, stroke, diabetes and many other health problems. Not everyone that snores has sleep apnea and not everyone that has sleep apnea snores. However, snoring is a warning sign and you should have your dentist or physician examine you. Your doctor may determine a asleep test is appropriate. Your dentist is an expert in the airway and can create an oral appliance that may alleviate the snoring.
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea is a common and serious sleep disorder that causes you to stop breathing during sleep. Sleep apnea affects a staggering number of Americans: 1 in 5 adults has mild OSA (obstructive sleep apnea) and 1 in 15 has moderate to severe OSA. Possibly 60 million Americans could be living with undiagnosed OSA and not even know it.
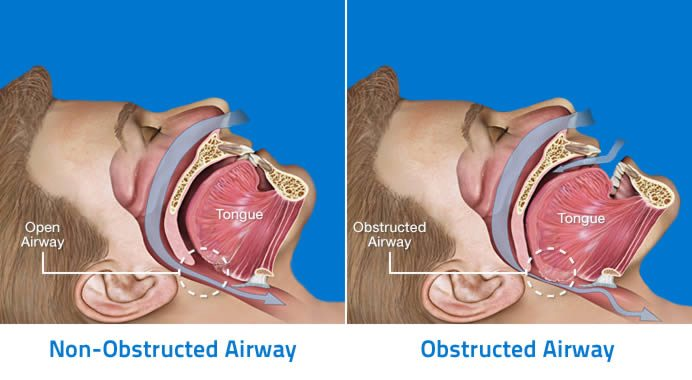
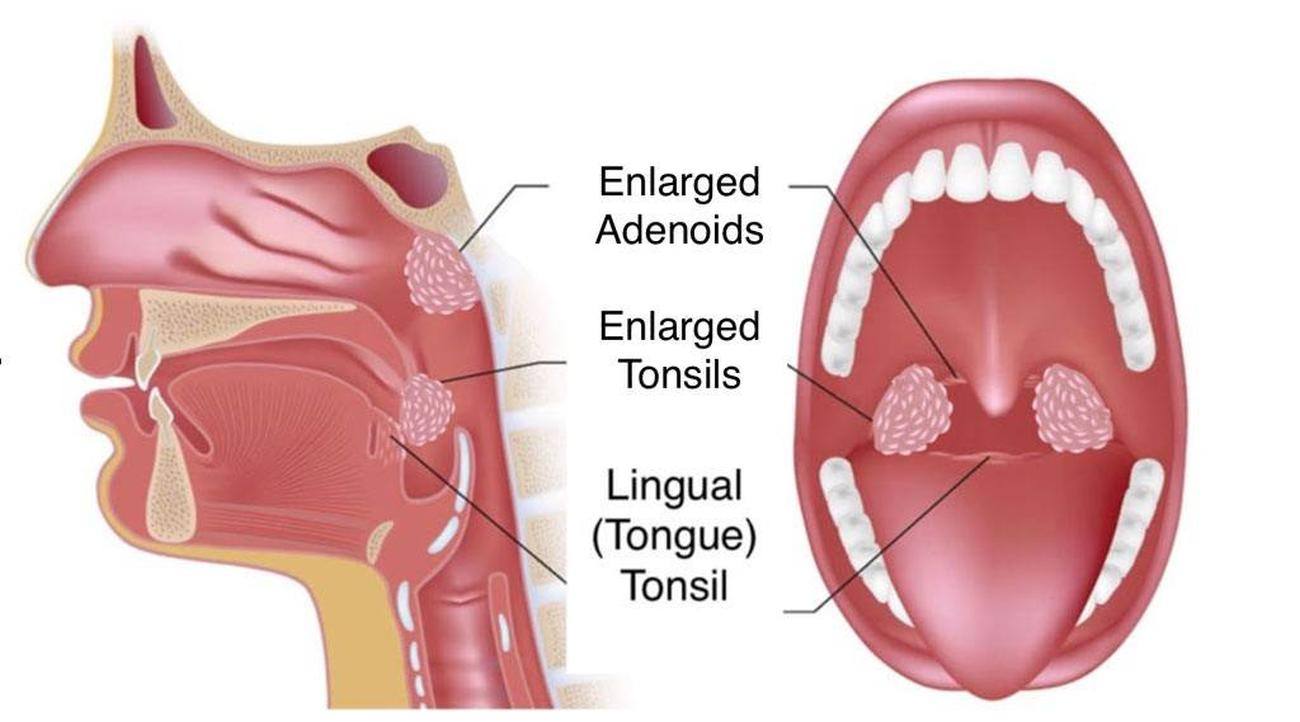
With OSA, the airway repeatedly becomes blocked, limiting the amount of air that reaches your lungs. A temporary pause in breathing is called an apnea. When this happens, you may snore loudly or making choking noises as you try to breathe. Your brain and body become oxygen deprived and you may wake up. This may happen a few times a night, or in more severe cases, several hundred times a night.The muscles of the upper airway relax when you fall asleep. If you sleep on your back, gravity can cause the tongue to fall back. This narrows the airway, which reduces the amount of air that can reach your lungs, and the narrowed airway also may cause snoring.
Sleep apnea can make you wake up in the morning feeling tired or unrefreshed even though you have had a full night of sleep. During the day, you may feel fatigued, have difficulty concentrating or you may even unintentionally fall asleep. This is because your body is waking up numerous times throughout the night, even though you might not be conscious of each awakening.
The lack of oxygen your body receives can have negative long-term consequences for your health.
This includes:
- High blood pressure
- Heart disease
- Stroke
- Pre-diabetes and diabetes
- Depression
[1] Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM., Am J Epidemiol. 2013 May 1;177(9):1006-14. doi: 10.1093/aje/kws342. Epub 2013 Apr 14
Risk Factors
The biggest risk factor for sleep apnea is excess body weight. You are much more likely to have OSA if you are overweight or obese, though it can occur in slim people too. According to the American Academy of Sleep Medicine common risk factors include:
- Excess weight – Your risk for sleep apnea is higher if you are overweight with a body mass index (BMI) of 25 or more or obese with a BMI of 30 or higher.
- Large neck size – Your risk for sleep apnea is higher if you have a neck size of 17 inches or more for men, or 16 inches or more for women. A large neck has more soft tissue that can block your airway during sleep.
- Middle age – Sleep apnea can occur at any age. However, it is more common between young adulthood and middle age.
- Male gender – Sleep apnea is more common in men than in women. For women the risk of sleep apnea increases with menopause.
- Hypertension – High blood pressure is extremely common in people who have sleep apnea.
- Family history – Sleep apnea is a heritable condition. This means that you have a higher risk of sleep apnea if a family member also has it. Inherited traits that increase the risk for sleep apnea include obesity and physical features such as a recessed jaw. Other common family factors – such as physical activity and eating habits – also may play a role.
Treating Snoring and Obstructive Sleep Apnea
Depending on the severity of your snoring and other symptoms, your doctor may want to conduct a sleep study. Sleep studies may sometimes be done at home. To treat your snoring, your doctor likely will first recommend lifestyle changes, such as:
- Losing weight
- Avoiding alcohol close to bedtime
- Treating nasal congestion
- Avoiding sleep deprivation
- Avoiding sleeping on your back
Dentists are experts in your oral cavity and airway. Across the country, many dentists are prepared to provide oral appliance therapy (link to OA below) to treat snoring. Rest Assured Technologies has a proven screening tool dentists use to determine if you are at risk for OSA. You should talk to your doctor and dentist about your treatment options.
Generally speaking, there are three ways to treat obstructive sleep apnea (OSA), and sometimes they are used to treat snoring also. These treatment options vary in their invasiveness and effect.
Surgery
- Prohibitive cost
- Any surgery carries risk & can lead to a painful recovery lasting 2-3 weeks
- May require time off of work
- Not guaranteed to cure sleep apnea (about 25 to 30% success rate)
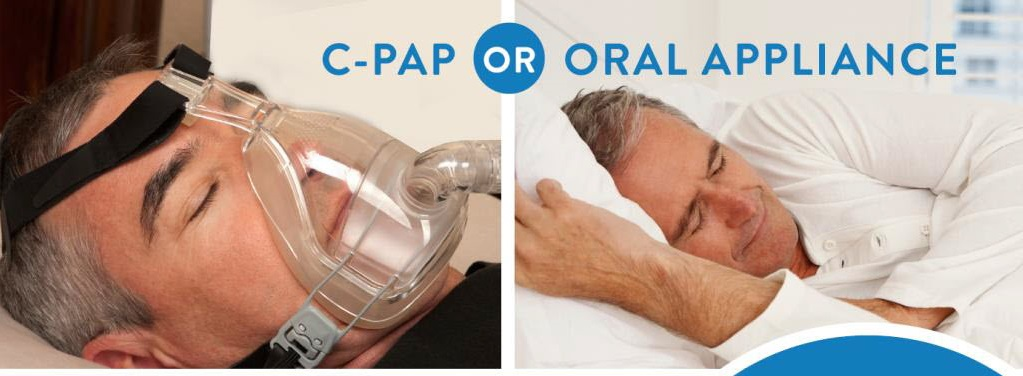
CPAP
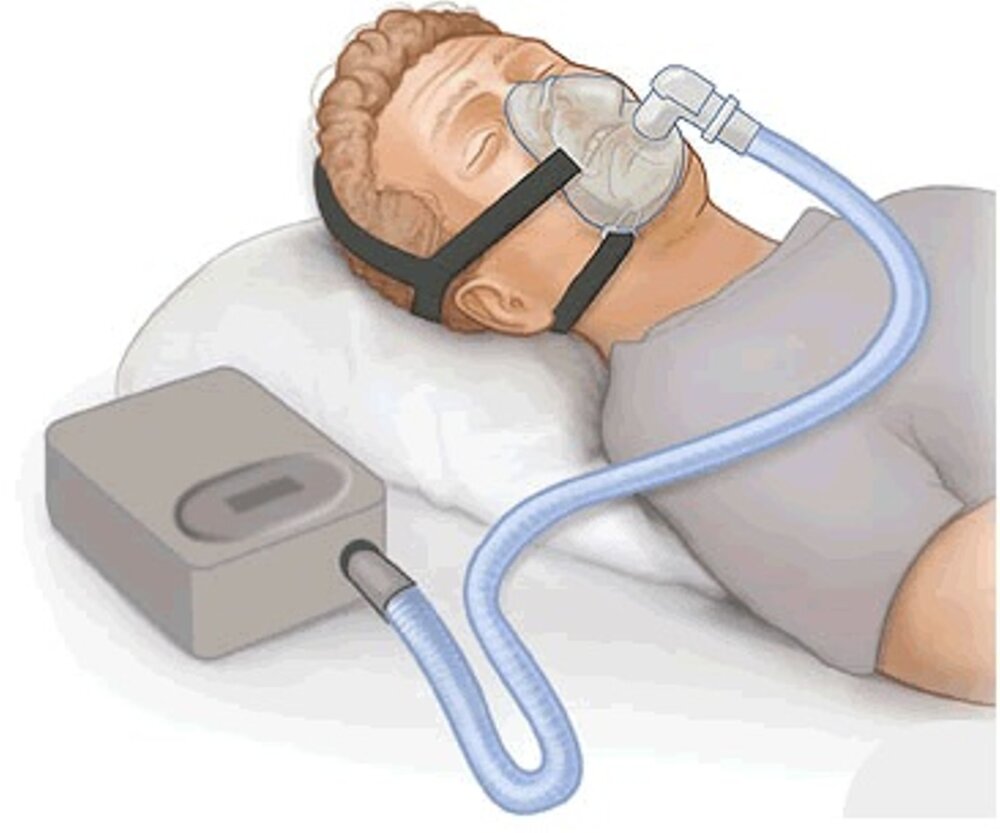
The most common treatment for sleep apnea is continuous positive airway pressure (CPAP) therapy. The CPAP machine keeps your airway open by providing forced air through flexible tubing and a required mask as you sleep. Although CPAP therapy is effective, it is expensive and some people are unable to adhere to it. In fact, it’s estimated that only 17% of CPAP users wear the device more than 4 hours per night.
- Expense of cumbersome mask & machine
- Ongoing CPAP maintenance (cleaning) & parts
- Low compliance rate
- May disturb bed partner
- Often more intensive treatment than required
- In-home sleep testing
- Lower cost than CPAP & Surgery
- High compliance rate
- Ongoing treatment can be provided with regular cleanings
Oral Appliance Therapy
Even with these issues, CPAP therapy is considered the “gold standard” for treating OSA by most medical doctors and insurance companies. Unfortunately, this is because many PCPs are not familiar with the success of oral appliance therapy. Your doctor should consider giving you a prescription for a sleep apnea appliance if you are unable to tolerate CPAP therapy or prefer an alternate treatment.
[3] The objective mean use rate was 6.4 +- 1.7 h/night at 1 year follow-up in continuing users, with a regular use rate of 83%. Dieltjens M, et al. Chest. 2013 Nov;144(5):1495-1502. doi: 10.1378/Chest.13-0613.
[4] Comparable effectiveness of OAm and CPAP has been attributed to higher reported nightly use of OAm. Sutherland K, et al., Oral Appliance Treatment for Obstructive Sleep Apnea: An Update. J Clin Sleep Med. 2014 Feb 15; 10(2): 215–227